Last Updated on 19 mins by Publishing Team
COVID-19 Update
Wednesday 30th March
| Transmission Update:
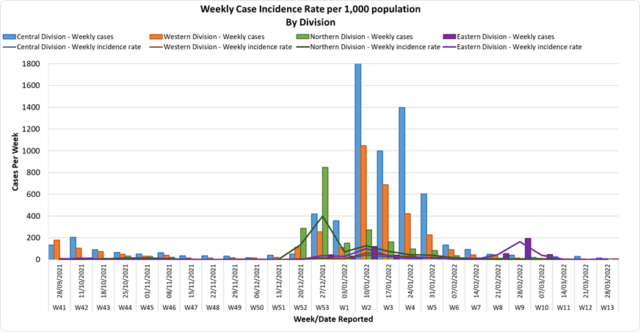
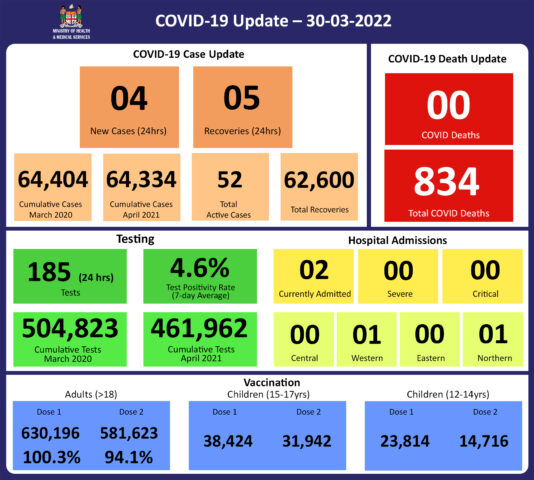
Since the last update, we have recorded 10 new cases of which 6 new cases were recorded on 29/03/2022 and 4 new cases in the last 24 hours ending at 8 am this morning. Of the 10 cases recorded, 8 cases were recorded in the Central Division; 2 cases were recorded in the Western Division, nil case was recorded in the Northern Division and the Eastern Division. The national 7-day rolling average of cases as of 26th March is 5 daily cases. In the 7 days until 29/03/2022, 16 new cases were recorded in the Central division, 9 new cases in the Western division, 5 new cases in the Northern Division, and 6 new cases in the Eastern Division. The Central Division cases constitute 68% of the cumulative total cases nationally, with the Western division making up 27%, 3% in the Northern Division, and 2% in the Eastern Division. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Deaths:
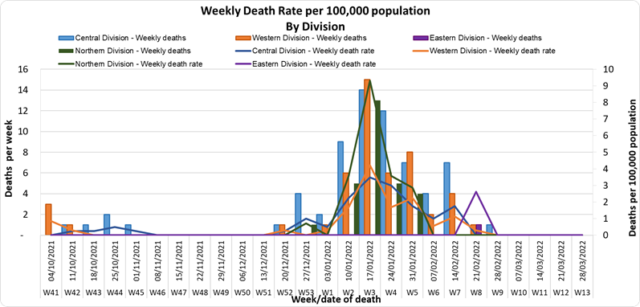
The curves depict weekly COVID-19 deaths by division since May 2021. It indicates a surge from December-end 2021, which peaks by mid-January 2022. The 3rd COVID 19 wave is considered to have started around mid to late December 2021. (Note: Death notifications from within the last two weeks are still being received, therefore the graphs may alter slightly upon reporting). Analysis of Deaths in the Third Wave Table 1: Death rates by Division
An analysis of the 138 deaths recorded in the third wave show that, while the Central Division has the highest absolute number of deaths, the Northern Division has the highest rate of death when adjusted for population. Table 2: Deaths by Age Group
For the 138 deaths in the third wave, the death rate adjusted per 100,000 population, has been highest in age groups 50 and onwards. There were 8 deaths below the age of 19 years, 7 out of the 8 children had significant pre-existing medical conditions, and one child had no known underlying medical condition. Table 3: Deaths by Vaccination Status
Out of 138 COVID -19 deaths reported in the third wave, six (6) deaths were in the population not eligible for vaccination (under age 12). An analysis of the 133 deaths in the vaccine-eligible population reflected, that when adjusted per 100,000 population, for fully vaccinated (received 2 doses) and unvaccinated/not fully vaccinated (received 0 doses or only 1 dose) adults in Fiji, a death rate of 9.6 per 100,000 population for fully vaccinated adults and 190.5 for unvaccinated adults was exhibited. This means that unvaccinated adults in Fiji have been dying at a rate 18.5 times higher than fully vaccinated adults during the current COVID-19 wave. Individuals of the 12-17 age group who died were not vaccinated. There have been no COVID-19 deaths in individuals who received a booster (3rd dose) of the vaccine. New deaths to report There is no new COVID-19 death to report. There have been a total of 834 deaths due to COVID-19 in Fiji. Please note that due to the time required by clinical teams to investigate, classify and report deaths, a 4-day interval is given to calculate the 7 days rolling average of deaths, based on the date of death, to help ensure the data collected is complete before the average is reported. Therefore, as of March 24th, 2022, the national 7 days rolling average for COVID-19 deaths per day is now 0.0, with a case fatality rate of 1.29%. We have recorded 916 COVID-19 positive patients who died from other serious medical conditions unrelated to COVID-19; their doctors determined that COVID-19 did not contribute to their deaths, therefore these are not classified as COVID-19 deaths. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Hospitalization:
There is a sustained downward trend in daily hospitalizations. Using the WHO clinical severity classification, 50% (n=1) are categorised as asymptomatic and mild, 50% (n=1) are categorised as moderate with nil cases in the severe and critical categories. Anyone admitted to the hospital is tested before admission, therefore, a significant number of people are admitted to the hospital for non-covid health conditions, but incidentally, test positive due to the high amount of transmission in the community. The number of people being admitted because of COVID-19 remains low. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Testing:
185 tests have been reported for March 29th, 2022. Total cumulative tests since 2020 are 504,823 tests. The 7-day daily test average is 143 tests per day or 0.2 tests per 1,000 population. The national 7-day average daily test positivity is 4.6%, which is within the WHO recommendation of 5%. |
Public Advisory:
Engaging COVID safety without mandates or quarantine
The recent announcements by the Honourable Minister for Economy in relation to COVID-19 represent a change in the phase of our engagement in the promotion of COVID-safe measures. We have been using mandates on masking and other protective restrictions over the last two years to institute COVID-safe measures, thereby slowing transmission and protecting the vulnerable. However, now that we have a high two-dose vaccination coverage, and booster doses have been readily available for months, we recognize that at some point everyone must take individual responsibility for keeping themselves safe with the measures that are available and known to be effective. We currently are recording low numbers of cases and admissions in our hospitals. And we have not recorded a new COVID-19 death for an entire month. Therefore, we now leave it to you to assess your own level of risk and decide to continue to take measures such as masking and social distancing. For example, we know wearing a mask in public will lower your risk of getting infected, and it is now an individual choice that is recommended by the Ministry. If you are at higher risk of severe disease should you get infected with COVID-19, we strongly recommend that you continue to wear a mask in public, particularly in crowded indoor spaces.
The lifting of masking and other mandates, and easing of travel restrictions, is NOT a sign that the risk of outbreak and resurgence of COVID-19 is over. It is only a reflection of MOHMS ‘appreciation that all that can be done to engage the community to live safely with the risk of COVID-19 has been done. The impact of COVID-19 has been seen and the results of collective response have been experienced and reported.
The promotion of COVID-safe measures will now be pursued similar to how we advise healthy lifestyle measures for the prevention of non-communicable diseases, and how basic hygiene is promoted for the prevention of infectious diseases like typhoid fever. The measures that will continue in terms of prevention are the promotion of vaccination, personal COVID-safe hygiene habits, and workplace ventilation and air cleaning measures. We recommend everyone continue to employ COVID-safe measures to prevent infection and the spread of infection: Frequently wash your hands or use an alcohol-based hand sanitizer, stay home if you feel sick, cover your mouth and nose with a tissue or the bend of your elbow if you cough or sneeze, wear a mask if you have any signs of a respiratory illness.
However, while we are now moving towards individual responsibility, we will keep in reserve the ability to reinstitute collective action in the future. The unfortunate fact is, that while many in Fiji and around the world are tired of COVID-19, the virus is not yet tired of us. Wishing it would go away will not make it a reality. The resurgence in COVID-19 in other countries is again a reminder of this fact. COVID is endemic to Fiji and is present in almost every country in the world, and as such the risk of resurgence will continue, with the highest risk to the unvaccinated, those with waning immunity, and those who have not had a vaccine booster dose. More importantly, the vulnerable among us will be susceptible to severe disease and death (even if they are vaccinated) when compared to the non-vulnerable group. Also, the non-vulnerable and mobile (e.g. young adults and adolescents) will always be able to transmit disease to the vulnerable. We expect that with the upcoming general elections, population mixing will be unavoidable.
A key part of the MOHMS strategy, moving forward will be to concentrate on health facilities and health care provision capabilities so as to mitigate against severe disease and death. This will include the ongoing community engagement and outreach program to facilitate early diagnosis and treatment in the community, and the maintenance of health facility readiness to provide treatment. Our command centres and operation centres have been repurposed to maintain a line list of vulnerable cases in the community and to work on processes that will allow for more preemptive response and promote broader community resilience. These command centres and operation centres will also provide oversight on community surveillance indicators to ensure early and measured responses to future outbreaks.
COVID-19 Vaccination
As of 30th March, a total of 117,059 individuals have so far received booster doses. While members of the public have been advised to obtain their booster dose after at least 5 months from their second COVID-19 vaccine dose, we will shortly be advising a shorter interval period in recognition of the risk of disease surge. Moderna vaccine and Pfizer vaccines are both available for adult booster doses.
The public is urged to get booster vaccine doses, and the list of vaccination sites is provided daily on the MOH webpage. The booster dose has been approved for deployment at a reduced post-dose 2 interval of 3 months compared to 5 months before. Given the competing issues, I have instructed teams to go back to health facilities and do targeted booster programs for the vulnerable and the willing and to focus on our 12 to 18-year-olds through the school vaccination program. Furthermore, we can confirm that we have accepted an offer of 50,000 doses of Pfizer Paediatric doses by the Aotearoa New Zealand Government as part of discussions with their Minister of Foreign Affairs, Nanaia Mahuta. Our team led by Dr. Tudravu is currently discussing with counterparts in NZ on further details. while our efforts to source more through our other development partners are ongoing.
Our school vaccination program has also been progressing such that with the 94% adult coverage rates, 88% of all persons over 12 years have had 2 doses of our COVID 19 vaccine.
We will continue to monitor the evidence on post-infection immunity based on quality data that is being generated globally. However, until we have a better sense of the role of post-infection immunity, the Ministry of Health will continue to define our level of protection based on vaccination numbers
Given the current stocks of Pfizer vaccine we have, we will be using Pfizer for the ongoing primary 2 dose schedule for children and adults and as the booster dose.
Surge Update
We are beginning to see a reduction in people presenting to health centres with acute respiratory illness, suspected leptospirosis, and suspected dengue fever, suggesting reductions in the current surge in outpatient cases. These declining trends of leptospirosis and dengue fever, despite the persistence of weather conditions conducive to their ongoing spread, is likely a result of the related public health measures that have been put in place. However, there remains the risk of disease resurgence if public health measures taken are not maintained.
The decline in cases has reduced the strain on our outpatient services, however, the Ministry will continue to work on measures to open more facilities with extended service hours, and streamline outpatient services to help reduce waiting times. Many of our staff have returned from annual leave that had been deferred during the second and third waves of COVID-19, as well as sick leave during the recent increase in influenza. Also, adjustments have been completed in our outreach programs to deal with LTDD, and vaccination needs and staff have been freed up for outpatients services in health centres.
The Ministry is working with the Ministry of Economy in pursuing the engagement of General Practitioners, Private Dental Practitioners, and Private Medical Laboratories, to provide and support outpatient services to the general public in a public-private partnership arrangement. We see this engagement as a key strategy to improve surge capacity support.
Leptospirosis, Typhoid fever, and Dengue fever
The current wet weather around the country continues to promote the surge of our endemic climate-sensitive diseases, leptospirosis, typhoid, and dengue fever. Though we have noted a decrease in leptospirosis hospital admissions, we are also aware of continued heavy rain in parts of the country, particularly the Western Division. As such the medical advice we provide needs to be followed, while we continue to mount our public health and clinical response. Please heed our advice to protect yourselves and your loved ones.
The 7-day Typhoid lockdown operation has been completed. During this time
- The targeted population in Togovere village was screened and treated.
- The main water supply and the water supply system to the individual houses were improved with each household in the village given a filter bucket for safe drinking water. The western health team also helped provide a 10,000L tank to help cater for water during dry spells.
- Sanitation facilities in the villages were assessed and improved with a total of 18 field latrines provided.
- Awareness of LTDs and WASH was conducted
- Sick patients were identified early and referred for admission and appropriate care
- The social welfare office together with the fisheries department had assisted the village. The teams had gathered the villagers shopping lists and money and did their shopping for them. They assisted 66 families by providing them with food and supplies from the supermarkets.
We acknowledge the effort and commitment demonstrated by the village leaders and community members in seeking, and complying with the lockdown initiative. We also acknowledge the coordinated response we had from the Roko Tui Ra and the Office of the Provincial Administrator Ra, Police, Ministry of Education, Ministry of Social welfare, Ministry of Fisheries, and Water Authority of Fiji’s rural water support initiative, Give Clean Water Fiji and UNICEF. This coordinated response was the key to the successful and timely completion of all the initiatives needed to mitigate the current outbreak in Togovere. The responsibility is now with the village community to protect themselves through good hands, food water, and sanitation hygiene practices.
Further data and updates on LTDD will be provided every Wednesday.
Leptospirosis
Prevention
The leptospirosis bacteria is spread to humans through the urine of infected animals, such as cows, pigs, rats, and dogs. To reduce your individual risk, it is important to understand that exposure to animals, soil, mud, and floodwaters during work or recreational activities increases your risk of infection.
Important prevention measures include wearing full covered footwear at all times when going outdoors, avoiding wading or swimming in flooded waters, using clean fresh water to wash up after exposure to muddy waters, and keeping all food and drinks covered and away from rats. For workplaces, practice good personal hygiene at all times, cover cuts and wounds well, and use protective equipment, especially footwear when in flooded and/or muddy areas.
We are also urging all parents and guardians to prevent children from playing in the mud or swimming in flooded rivers or creeks, and ensure that they wear shoes when outside.
Symptoms and treatment
Early treatment can decrease the severity and duration of the disease. Please seek medical care if you have recently had contact with floodwaters, mud, or animals, and develop the following symptoms: fever, muscle pain, headache. You may also have red eyes, loss of appetite, nausea/vomiting, dizziness, or feel weak.
Leptospirosis can be treated with appropriate antibiotic medications prescribed by a doctor if treatment is sought early. Danger signs for severe leptospirosis include shortness of breath, coughing blood, chest pain, yellow eyes/skin (jaundice), signs of bleeding (including unexplained bruising), decreased or increased urination, difficulty staying awake. Severe leptospirosis is life-threatening, and anyone with these symptoms must be taken to the hospital immediately.
The reports from the recent FEMAT outbreak response visits to the Navosa Subdivision and the Ra Subdivision have shown that when patients are seen early, and the appropriate treatment was provided, the patients were able to be treated successfully at home and did not require admissions into the hospital. The number of people with severe disease and deaths was all significantly reduced. Therefore, we encourage those who are sick at home to seek treatment early so they can recover quickly from their illness.
Typhoid fever
Typhoid fever is typically found in areas that do not have access to proper toilet facilities and/or clean drinking water. We strongly encourage people who live in rural areas, informal urban areas, and any other areas where access to clean drinking water is limited, to boil all drinking water. We must all also continue to practice basic hygiene measures such as frequently washing hands with soap and water, especially after visiting the toilet and before eating or preparing food.
The preliminary reports from our WASH projects in the Northern division have shown that when communities focus on ensuring good water supply, practising proper hand hygiene, having proper human waste disposal (hygienic toilet facilities), and complete treatment of those with the disease, outbreaks of typhoid can be stopped in the community; and the overall prevalence of typhoid fever will decrease. Thus, we encourage all our communities to focus on clean and hygienic WASH facilities to stop the spread of typhoid fever in the community.
Dengue fever
We continue to urge everyone to get rid of potential mosquito breeding places, such as empty containers inside and outside your homes that may collect water, including discarded tires, flower vases, and pot plant bases. Protect yourself from being bitten by mosquitoes by using mosquito screens in your home, and mosquito repellents.