Last Updated on 15 hours by Publishing Team
COVID-19 Update
Monday 16th May
Public Advisory
Engaging COVID safety without mandates or quarantine
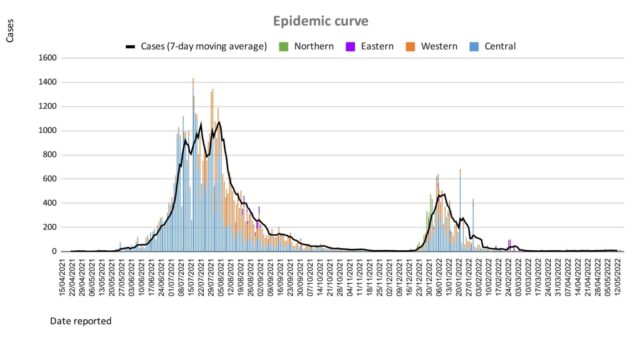
Since the 7th of April and the lifting of our quarantine measures and increased international travel, our community and border surveillance screening data continue to report a low positivity rate despite the ongoing pandemic, and the continued evolution of Omicron variants. While there is a low positivity rate among arrivals we are seeing positive arrivals. We are also aware that a key aspect of living with Covid is to have a strong community surveillance system within the community AND at the border. This will allow early identification of community outbreaks and facilitate early response. Early response capability is a key part of mitigating the risk of severe disease and severe containment measures and to further easing pre-departure conditions for international travel. As part of our community surveillance exercise, we will be transitioning to t9he more routine use of throat and nasal swabs as opposed to the more uncomfortable nasopharyngeal swabs
The Ministry informs the public that for the positive cases among arrivals, existing protocols have been instituted to ensure travellers that return positive COVID-19 test results follow protocols and isolate for the required 7 – days as advised.
However, the Ministry is concerned that there are travellers who are not adhering to the 7-days of isolation and continue to be mobile during that 7-day isolation period.
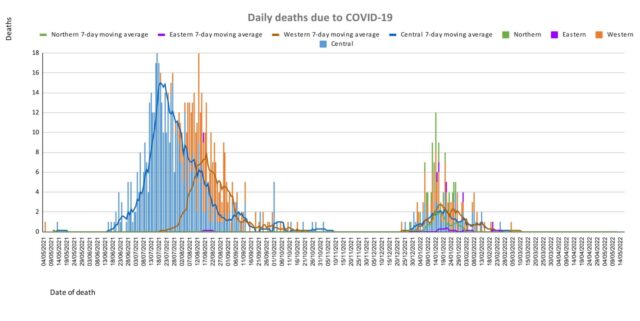
We call on the public to support the protection and safety of all Fijians by reminding travellers from overseas who are visiting friends and relatives of the importance of isolating themselves for 7 days if they test positive for COVID-19. As a nation, Fiji has emerged from the period of restrictions that were instituted to protect our people and our country from COVID-19. We need not be reminded of the high number of positive cases and the number of deaths from COVID-19. The Ministry reiterates that the lifting of masking and other mandates and easing of travel restrictions is NOT a sign that the risk of outbreak and resurgence of COVID-19 is over. It is important that we continue to work together to protect ourselves, our communities and our country from any further
The following prevention measures continue; the promotion of vaccination, personal COVID-safe hygiene habits, and workplace ventilation and air cleaning measures. We recommend everyone continue to employ COVID-safe measures to prevent infection and the spread of infection: Frequently wash your hands or use an alcohol-based hand sanitiser, stay home if you feel sick, cover your mouth and nose with a tissue or the bend of your elbow if you cough or sneeze, wear a mask if you have any signs of a respiratory illness.
We have dropped the pre-departure testing requirement for travellers coming into Fiji and also we now require international arrivals to test within 72 hours of arrival. Beyond this potential change, our border protection will be mediated by the fact that all travellers over 16 years are vaccinated. Inbound travellers aged 12 years and above must produce proof of a pre-booked and pre-paid rapid antigen test, to be administered within 72 hours of arrival in Fiji. Booking for tests can be made through this link: https://entrytestfiji.com. There will be exemptions for those who have tested positive and recovered from COVID-19 within the 30 days before travel and have fit-to-fly certificates. Failure to comply with arrival testing once in Fiji will result in a spot fine of $1000.
Ongoing Medical Recovery Efforts
With the reduction in COVID-19 cases and in people presenting to health centres with acute respiratory illness, the MOHMS team is better positioned to focus more on health facilities and health care provision capabilities to mitigate against severe disease and death. This will include the ongoing community engagement and outreach program to facilitate early diagnosis and treatment in the community, and the maintenance of health facility readiness to provide treatment.
Our command centres and operation centres have been repurposed to maintain a line list of vulnerable cases in the community and to work on processes that will allow for more preemptive response and promote broader community resilience. These command centres and operation centres will also provide oversight on community surveillance indicators to ensure early and measured responses to future outbreaks.
We are also focused on carrying out general health service work more efficiently in all facilities, and a key part of our plan is to set up divisional mobile units to supplement facility-based general servicing capability and also work with private providers through a process for pre-qualifying contractors and/or suppliers for each subdivision.
The engagement of General Practitioners, Private Dental Practitioners, Private Medical Laboratories, and Private Ambulance providers to support our services in a public-private partnership arrangement is a strategy to help in our ongoing recovery efforts.
We also have reformulated a framework to better engage customer service initiatives in all health facilities and allow for senior managers to institute substantive actions and provide direct oversight over implementation plans. It will also allow the Ministry’s senior executives to track progress in implementation and ensure that annual operation plans reflect an evolving and progressive change narrative in the successive plans. These initiatives will also include the processing of internal communications to facilitate timely decision making and action within the Ministry.
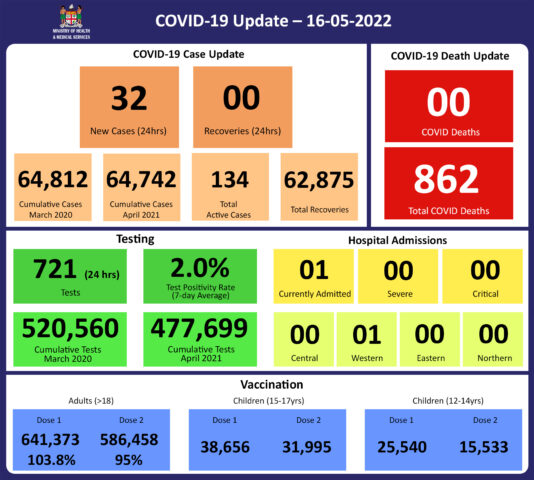
COVID-19 Vaccination
As of the 16th of May, a total of 126,926 individuals have so far received booster doses. This represents 29.5% of those eligible for a booster dose. The booster dose interval for eligible persons has been reduced to 3 months from the 2nd dose. This is in recognition of the risk of disease surge based on waning 2 doses covid vaccine protection, slow booster uptake, increased international travel with the relaxation of border measures, and ongoing outbreaks in various parts of the world. Moderna vaccine and Pfizer vaccines are both available for adult booster doses.
The public is urged to get booster vaccine doses, and the list of vaccination sites is provided daily on the MOH. We have accepted an offer of 50,000 doses of Pfizer paediatric doses for children aged 5 to 11 by the Aotearoa New Zealand Government. Our vaccination team is currently discussing with counterparts in NZ on further details while our efforts to source more through our other development partners are ongoing.
Our school vaccination program has also been progressing such that with the 95% adult coverage rate, 90.6% of all persons over 12 years have had 2 doses of the COVID-19 vaccine.
We will continue to monitor the evidence on post-infection immunity based on quality data generated globally. However, until we have a better sense of the role of post-infection immunity, the Ministry of Health will continue to define our level of protection based on vaccination numbers
Given the current stocks of Pfizer vaccines, we are now covering the Primary doses for those yet to be vaccinated and for Dose 2 if individuals were vaccinated with either Moderna or Astra Zeneca while the 12-14-year-olds continue with the Pfizer vaccine. The new supplies of MODERNA are expected to be available in-country at the end of the month.
Leptospirosis
There have been 2068 lab-confirmed cases of leptospirosis this year, with 111 new cases to report since the last update. A slight upward trend in cases with case numbers is noted above the outbreak threshold nationally, driven by cases in the Western Division. Case numbers are above the expected numbers for this time of the year.
Case numbers in the Western Division are increasing and remain above the outbreak alert threshold, indicating more cases than the expected number for this time of the year for this endemic disease. In the West, there have been 864 lab-confirmed cases, with 54 new cases since the last update.
In the Central Division, there have been 715 cases, with 29 new cases since the last update. Case numbers have increased towards the outbreak alert threshold in the last two weeks in Central..
In the Northern Division, there have been 427 cases, with 27 new cases since the last update. Case numbers have risen above the outbreak alert threshold in the last week, and are just above the average number of cases expected at this time of the year.
In the Eastern Division, there have been 62 cases, with 1 new case reported since the last update. Case numbers have continued to remain below the outbreak alert threshold and are at the average number seen at this time of the year.
For national leptospirosis hospital admissions so far this year, there have been 681 people admitted in total- noting that this includes suspected and lab-confirmed cases. Total leptospirosis hospital admissions this year by division are as follows:
- 380 people have been admitted to the hospital for leptospirosis in the West, with 14 new admissions last week, indicating a plateau in the trend compared to the previous week.
- 179 people have been admitted to the hospital for leptospirosis in Central with 5 new admissions last week, a plateauing trend compared to the admissions in the previous week. There have been 4-5 admissions a week in Central over the last 4 weeks.
- 103 people have been admitted to the hospital for leptospirosis in the Northern Division, with 1 new admission in the last week, which is a decrease in the admission trend compared to the 8 admissions in the week before.
- 19 people have been admitted to the hospital in the Eastern Division, with no new admissions since the last update.
Sadly, there are 5 new leptospirosis deaths to report since the last update on April 25th, the details of the people who died are as follows:
39-year-old male from Qamea who was admitted to CWM Hospital on April 30th, and died on 03/05/22.
31-year-old male from Ba who died at home or en-route to hospital on 02/05/22
41-year-old male from Lautoka who was admitted and died at Lautoka Hospital on 19/04/22
50-year-old male from Ba who was admitted at Lautoka hospital on 20/04/22 and died on 21/04/22
16 year old from Ba who was admitted at died at Lautoka Hospital on 13/04/22
There have been a total of 41 deaths from leptospirosis this year, with 30 in the Western Division, 4 in Central, 6 in the North, and 1 in the Eastern Division.
Prevention
The leptospirosis bacteria is spread to humans through the urine of infected animals, such as cows, pigs, rats, and dogs. To reduce your individual risk, it is important to understand that exposure to animals, soil, mud, and floodwaters during work or recreational activities increases your risk of infection.
Important prevention measures include wearing full covered footwear at all times when going outdoors, avoiding wading or swimming in flooded waters, using clean fresh water to wash up after exposure to muddy waters, and keeping all food and drinks covered and away from rats. For workplaces, practice good personal hygiene at all times, cover cuts and wounds well, and use protective equipment, especially footwear when in flooded and/or muddy areas.
We are also urging all parents and guardians to prevent children from playing in the mud or swimming in flooded rivers or creeks, and ensure that they wear shoes when outside.
Symptoms and treatment
Early treatment can decrease the severity and duration of the disease. Please seek medical care if you have recently had contact with floodwaters, mud, or animals, and develop the following symptoms: fever, muscle pain, or headache. You may also have red eyes, loss of appetite, nausea/vomiting, dizziness, or feel weak.
Leptospirosis can be treated with appropriate antibiotic medications prescribed by a doctor if treatment is sought early. Danger signs for severe leptospirosis include shortness of breath, coughing blood, chest pain, yellow eyes/skin (jaundice), signs of bleeding (including unexplained bruising), decreased or increased urination, and difficulty staying awake. Severe leptospirosis is life-threatening, and anyone with these symptoms must be taken to the hospital immediately.
Typhoid fever
There have been 116 lab-confirmed cases of typhoid fever this year, with 5 new cases since the last update.. Case numbers at the national level, and in the 4 divisions, are currently at the average level expected at this time of the year for this endemic disease.
There have been no new deaths caused by typhoid fever since the last update. There have been 6 deaths confirmed to have been caused by typhoid fever this year.
Typhoid fever is typically found in areas that do not have access to proper toilet facilities and/or clean drinking water. We strongly encourage people who live in rural areas, informal urban areas, and any other areas where access to clean drinking water is limited, to boil all drinking water. We must all also continue to practice basic hygiene measures such as frequently washing hands with soap and water, especially after visiting the toilet and before eating or preparing food.
Dengue Fever
There have been 1960 lab-confirmed cases of dengue fever this year, with 92 new cases since the last update. Case numbers are below the average numbers seen at this time of the year nationally, as well as in the Central, Eastern, and Northern Divisions.
Case numbers in the Western Division are now below the outbreak alert threshold and at the expected level seen at this time of the year, though a slight upward trend has been noted in the last week. There have been 730 cases of dengue fever recorded in the Western Division this year.
We continue to urge everyone to get rid of potential mosquito breeding places, such as empty containers inside and outside your homes that may collect water, including discarded tires, flower vases, and pot plant bases. Protect yourself from being bitten by mosquitoes by using mosquito screens in your home, and mosquito repellents.
Cold and flu
The Ministry of Health and Medical Services has noted an increase in people becoming ill with cold and flu-like illnesses as we are coming into our dry and cold season. This increase is especially seen in infants and children under the age of 5. The paediatrics department at CWM Hospital is also seeing an increase in children under the age of 5, especially infants, being admitted with acute respiratory illnesses while testing negative for COVID-19 and influenza. It has been expected that as restrictions intended to prevent transmission of COVID-19 were lifted (including mandatory masking, physical distancing, and school and border closures) other respiratory viruses that normally circulate would begin to re-emerge similar to pre-COVID levels, and possibly even at higher levels due to a decrease in population immunity to seasonal viruses, as cold/flu cases were low during the last two years.
Care for children with cold and flu symptoms
Keep your child hydrated to reduce cold and flu symptoms and help them feel better. Fevers can result in dehydration. Your child may not feel as thirsty as they normally would, and they may be uncomfortable when drinking, so it is important to encourage them to drink plenty of fluids like fresh fruit juices and water (e.g. lemon juice).
Dehydration can be very serious in babies, especially if they’re under 3 months old. Go immediately to your nearest health centre or doctor if you suspect your baby is dehydrated. Some signs may include:
- no tears when crying
- dry lips
- a soft spot in the head that seems sunken-in
- decreased activity
- urinating less than three to four times in 24 hours
If your child is breastfed, attempt to breastfeed them more frequently than usual. Your baby may be less interested in breastfeeding if they’re sick. You may have to have several short feeding sessions or express breast milk and give in a small cup in order for them to consume enough fluid.
Clear up stuffed nasal passages and loosen mucous to ease cough
Careful use of a steam source in a closed room can help to relieve a stuffed nose and soften mucous to make coughing up mucous easier.
Saline drops for the nose can also be bought at pharmacies to soften nasal mucous and facilitate its discharge
Alternatively use a small amount of Vicks rub mixed with oil over the heels of feet for children >3 months old
If your child is over 1-year-old, try giving honey for a cough instead of medication. You can give 2 to 5 millilitres (mL) of honey a few times during the day.
Encourage rest
Extra rest can help your child recover faster.
Fever
Your child may be very hot due to fever. Dress them lightly and avoid heavy blankets or excessive layers that could make them feel hotter. A mild fever does not need treatment as fever is the body’s way of fighting off an infection. A lukewarm bath can also help them cool off and wind down before taking a nap or going to sleep for the night.
Seek medical care
Sometimes even the best at-home care isn’t enough to help your little one make a full recovery. Seek medical care right away if your child has any of the following:
- has a fever greater than 38°C for more than two days, or a fever of 40°C or higher for any amount of time
- has a fever of 38°C or higher and is under 3 months old
- has a fever that doesn’t get better after taking Panadol
- seems unusually drowsy or lethargic
- won’t eat or drink
- is wheezing or is short of breath
Prevention
After your child recovers, there are steps you can take to prevent cold and flu in the future. Wash all surfaces they came into contact with before or during their sickness. Encourage your children and other family members to wash their hands regularly to keep germs at bay.
Teach your child not to share food, drinks, or utensils when they eat. This assists in avoiding the spread of germs between them and their friends. Keep your child out of daycare or school when they are ill, especially if they have a fever. Keep them away from others with flu-like symptoms and avoid crowds.