Last Updated on 3 hours by Publishing Team
COVID-19 Update
Wednesday 06th April
| Transmission Update:
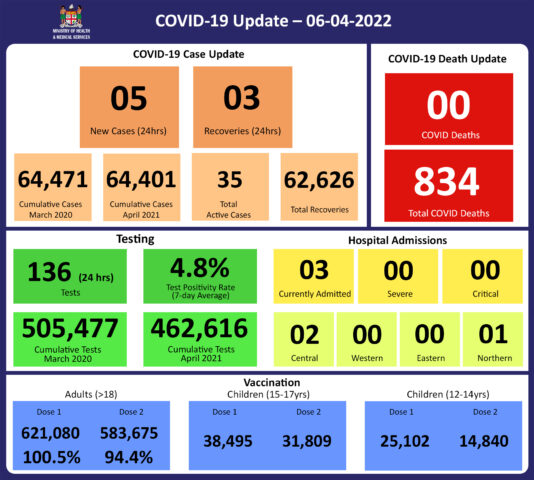
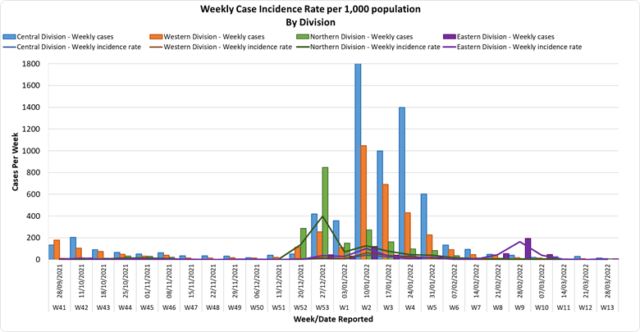
Since the last update, we have recorded 10 new cases of which 5 new cases were recorded on 05/04/2022 and 5 new cases in the last 24 hours ending at 8 am this morning. Of the 10 cases recorded, 3 cases were recorded in the Central Division; 7 cases were recorded in the Western Division while nil cases were recorded in the Northern Division and Eastern Division. The national 7-day rolling average of cases as of 2nd April is 4 daily cases. In the 7 days until 05/04/2022, 7 new cases were recorded in the Central division, 11 new cases in the Western division, 2 new cases in the Northern Division, and 1 new case in the Eastern Division. The Central Division cases constitute 68% of the cumulative total cases nationally, with the Western division making up 27%, 3% in the Northern Division, and 2% in the Eastern Division. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Deaths:
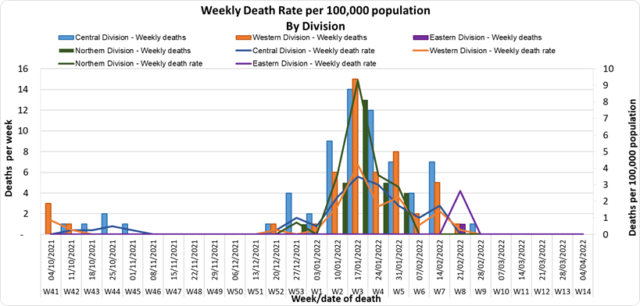
The curves depict daily COVID-19 deaths by division since May 2021. It indicates a surge from December-end 2021, which peaks by mid-January 2022. The 3rd COVID 19 wave is considered to have started around mid to late December 2021. (Note: Death notifications from within the last two weeks are still being received, therefore the graphs may alter slightly upon reporting). Analysis of Deaths in the Third Wave Table 1: Death rates by Division
An analysis of the 138 deaths recorded in the third wave shows that, while the Central Division has the highest absolute number of deaths, the Northern Division has the highest rate of death when adjusted for population. Table 2: Deaths by Age Group
For the 138 deaths in the third wave, the death rate adjusted per 100,000 population, has been highest in age groups 50 and onwards. There were 8 deaths below the age of 19 years, 7 out of the 8 children had significant pre-existing medical conditions, and one child had no known underlying medical condition. Table 3: Deaths by Vaccination Status
Out of 138 COVID -19 deaths reported in the third wave, six (6) deaths were in the population not eligible for vaccination (under age 12). An analysis of the 133 deaths in the vaccine-eligible population reflected, that when adjusted per 100,000 population, for fully vaccinated (received 2 doses) and unvaccinated/not fully vaccinated (received 0 doses or only 1 dose) adults in Fiji, a death rate of 9.6 per 100,000 population for fully vaccinated adults and 190.5 for unvaccinated adults was exhibited. This means that unvaccinated adults in Fiji have been dying at a rate 18.5 times higher than fully vaccinated adults during the current COVID-19 wave. Individuals of the 12-17 age group who died were not vaccinated. There have been no COVID-19 deaths in individuals who received a booster (3rd dose) of the vaccine. New deaths to report There is no new COVID-19 death to report. There have been a total of 834 deaths due to COVID-19 in Fiji. Please note that due to the time required by clinical teams to investigate, classify and report deaths, a 4-day interval is given to calculate the 7 days rolling average of deaths, based on the date of death, to help ensure the data collected is complete before the average is reported. Therefore, as of March 29th, 2022, the national 7 days rolling average for COVID-19 deaths per day is now 0.0, with a case fatality rate of 1.29%. We have recorded 922 COVID-19 positive patients who died from other serious medical conditions unrelated to COVID-19; their doctors determined that COVID-19 did not contribute to their deaths, therefore these are not classified as COVID-19 deaths. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Hospitalization:
There is a sustained downward trend in daily hospitalizations. Using the WHO clinical severity classification, 67% (n=2) are categorised as asymptomatic and mild; 33% (n=1) are categorised as moderate with nil cases in the severe and critical categories. Anyone admitted to the hospital is tested before admission, therefore, a significant number of people are admitted to the hospital for non-covid health conditions, but incidentally, test positive due to the high amount of transmission in the community. The number of people being admitted because of COVID-19 remains low. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Testing:
136 tests have been reported for April 5th, 2022. Total cumulative tests since 2020 are 505,477 tests. The 7-day daily test average is 93 tests per day or 0.1 tests per 1,000 population. The national 7-day average daily test positivity is 4.8%, which is within the WHO recommendation of 5%. |
Public Advisory
Engaging COVID safety without mandates or quarantine
As of the 7th of April, all quarantine measures are now lifted. Our border protection will be mediated by the fact that travellers are vaccinated, have a negative pre-departure test and will be tested in-country by a rapid antigen test done between 48 hours and 72 hours after the arrival. There will be exemptions for those with fit to fly certificates.
As such the onus is now, more firmly on the individual to keep themselves safe with the measures that are available and known to be effective. We leave it to you to assess your own level of risk and decide to continue to take measures such as masking and social distancing. For example, we know wearing a mask in public will lower your risk of getting infected, and it is now an individual choice that is recommended by the Ministry. If you are at higher risk of severe disease should you get infected with COVID-19, we strongly recommend that you continue to wear a mask in public, particularly in crowded indoor spaces.
The lifting of masking and other mandates, and easing of travel restrictions, is NOT a sign that the risk of outbreak and resurgence of COVID-19 is over. It is only a reflection of MOHMS ‘appreciation that all that can be done to engage the community to live safely with the risk of COVID-19 has been done. The impact of COVID-19 has been seen and the results of collective response have been experienced and reported.
The promotion of COVID-safe measures will now be pursued similar to how we advise healthy lifestyle measures for the prevention of non-communicable diseases, and how basic hygiene is promoted for the prevention of infectious diseases like typhoid fever. The measures that will continue in terms of prevention are the promotion of vaccination, personal COVID-safe hygiene habits, and workplace ventilation and air cleaning measures. We recommend everyone continue to employ COVID-safe measures to prevent infection and the spread of infection: Frequently wash your hands or use an alcohol-based hand sanitiser, stay home if you feel sick, cover your mouth and nose with a tissue or the bend of your elbow if you cough or sneeze, wear a mask if you have any signs of a respiratory illness.
However, while we are now moving towards individual responsibility, we will keep in reserve the ability to reinstitute collective action in the future. COVID is endemic to Fiji and is present in almost every country in the world, and as such the risk of resurgence will continue, with the highest risk to the unvaccinated, those with waning immunity, and those who have not had a vaccine booster dose. More importantly, the vulnerable among us will be susceptible to severe disease and death (even if they are vaccinated) when compared to the non-vulnerable group. Also, the non-vulnerable and mobile (e.g. young adults and adolescents) will always be able to transmit disease to the vulnerable. We expect that with the upcoming general elections, population mixing will be unavoidable.
Ongoing Medical Recovery Efforts
With the reduction in covid cases and reduction in people presenting to health centres with acute respiratory illness, the MOHMS team is in a better position to focus more on health facilities and health care provision capabilities so as to mitigate against severe disease and death. This will include the ongoing community engagement and outreach program to facilitate early diagnosis and treatment in the community, and the maintenance of health facility readiness to provide treatment. Our command centres and operation centres have been repurposed to maintain a line list of vulnerable cases in the community and to work on processes that will allow for more preemptive response and promote broader community resilience. These command centres and operation centres will also provide oversight on community surveillance indicators to ensure early and measured responses to future outbreaks.
A key focus is also on carrying out general service work more efficiently in all facilities. With the return of our much needed corporate staff, the process of reporting and prioritising general works, and ensuring they are communicated clearly and tracked through our command centre and operation will be improved. A key part of our plan is to set up divisional mobile units to supplement facility-based general servicing capability and also work with private providers through a process for pre-qualifying contractors and/or suppliers for each subdivision.
The engagement of General Practitioners, Private Dental Practitioners, Private Medical Laboratories, and Private Ambulance providers to support our services to the general public in a public-private partnership arrangement is also seen as a key strategy to help in our ongoing recovery efforts.
Surge Update
As mentioned, current data do indicate an increase in the recent week of suspected and confirmed cases of leptospirosis, and dengue fever. This trend is seen mostly in the Western division and is consistent with the high level of rainfall that is expected to persist over this weekend. The risk of disease resurgence and resulting in severe outcomes can only be mitigated by adherence to public health measures. The medical advice we provide needs to be followed, while we continue to mount our public health and clinical response. Please heed our advice to protect yourselves and your loved ones. We will be updating LTDD data and advice on Friday.
COVID-19 Vaccination
As of the 06th of April, a total of 119,402 individuals have so far received booster doses. The booster dose interval for eligible persons has been reduced. This is in recognition of the risk of disease surge based on waning 2 doses covid vaccine protection, slow booster uptake increased international travel with the relaxation of border measures and ongoing outbreaks in various parts of the world. We have provided advice for members of the public to obtain their booster dose after at least 3 months from their second COVID-19 vaccine dose. Moderna vaccine and Pfizer vaccines are both available for adult booster doses.
The public is urged to get booster vaccine doses, and the list of vaccination sites is provided daily on the MOH webpage. The booster dose has been approved for deployment at a reduced post-dose 2 interval of 3 months compared to 5 months before. Given the competing issues, I have instructed teams to go back to health facilities and do targeted booster programs for the vulnerable and the willing and to focus on our 12 to 18-year-olds through the school vaccination program. Furthermore, we can confirm that we have accepted an offer of 50,000 doses of Pfizer Paediatric doses by the Aotearoa New Zealand Government as part of discussions with their Minister of Foreign Affairs, Nanaia Mahuta. Our team led by Dr. Tudravu is currently discussing with counterparts in NZ on further details. while our efforts to source more through our other development partners are ongoing.
Our school vaccination program has also been progressing such that with the 94% adult coverage rates, 88% of all persons over 12 years have had 2 doses of the COVID 19 vaccine.
We will continue to monitor the evidence on post-infection immunity based on quality data that is being generated globally. However, until we have a better sense of the role of post-infection immunity, the Ministry of Health will continue to define our level of protection based on vaccination numbers
Given the current stocks of Pfizer vaccine we have, we will be using Pfizer for the ongoing primary 2 dose schedule for children and adults and as the booster dose.