Last Updated on 2 hours by Publishing Team
COVID-19 Situation Update
Saturday 01st January 2022
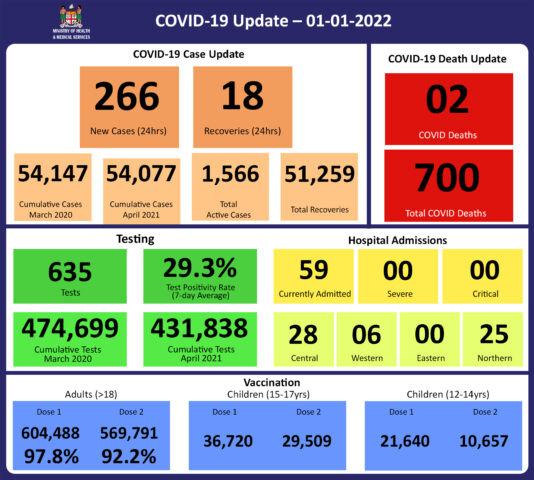
Tests
As of today, rapid antigen tests conducted in the Ministry of Health and Medical Services health facilities are being added to testing numbers and test positivity calculations going back to December 23rd. Prior to this, only PCR tests were reported, though recently, rapid antigen test positives were also reported, and used in test positivity calculations. Furthermore, negative PCR test results from one lab were not being received nor added to the test count, while their positives were being reported. As test positivity is calculated by dividing positive tests by total tests, this resulted in test positivity being reported as higher than the actual. This has now been corrected. Nevertheless, it should be noted that test positivity remains high and the trend of test positivity remains the same as it continues to increase along with case numbers.
Epidemic Outlook:
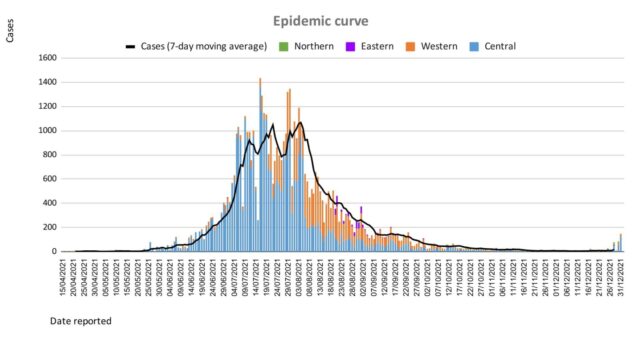
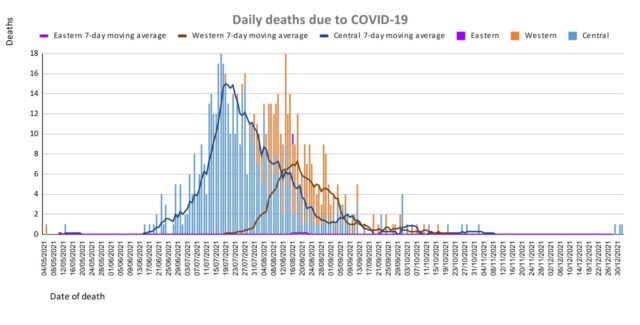
The Ministry of Health continues to monitor the outbreak using indicators such as daily case numbers, hospitalizations, test positivity, and deaths.
Occupancy rates in health facilities, the occupancy rate of ICU beds, death rates, and vaccination coverage are indicators to monitor our health response capacity. While we see a low trend across indicators from our health facilities with increasing vaccination coverage for adults, 15-17-year-olds, and 12-14-year-olds in Fiji the current escalation of cases indicates a need for increased readiness and response levels for severe disease and hospitalization.
COVID-19 cases are increasing rapidly globally and especially so in Australia, and the European and Americas region, and throughout Africa. The new highly transmissible variant Omicron is contributing significantly to this increase. As such, we anticipate an increasing number of cases from border quarantine facilities. Increased and sustained surveillance and testing at our borders, communities, and maritime islands are vital to monitor and detect COVID-19 cases for early intervention.
There is an increasing number of cases in all divisions which is anticipated to continue to increase, demanding ongoing surveillance for early intervention to mitigate COVID-19 risks.
Public Advisory:
The Ministry of Health and Medical Services has documented a resurgence in COVID-19 cases throughout Fiji while our hospitals are recording a lower than expected number of hospitalizations from the virus. The majority of individuals testing positive in medical facilities had presented for non-COVID medical problems and were found to be positive while undergoing routine screening as all admissions to the hospital are currently tested for COVID-19. It is likely that this is the impact of the vaccination and booster doses in preventing hospitalization, severe illness, and death. Our briefings have also revealed that almost all the cases turning positive have minimal symptoms and remain stable
Our contact tracing investigations reveal that the additional protection that vaccines provide against infection is evident. However, some recent events of excessive crowding in maritime vessels, sporting events, and social gatherings are proving to be superspreader events contributing significantly to the sharp surge in cases.
The overall goal of the MOHMS COVID-19 pandemic response and recovery is to suppress ongoing community transmission to a level that will minimize hospitalization, severe illness, and deaths, as well as minimize severe societal disruption. We are prioritizing the promotion of individual COVID safe measures (vaccination, masking, physical distancing, avoiding crowds, hand hygiene), followed by settings-based measures (social gathering restrictions, indoor capacity restrictions, ventilation, and curfews). We would like to avoid population blanket measures such as lockdowns, which we used earlier in this pandemic, as such measures have also negatively impacted our communities on other fronts. In our own recent experience, such measures have limited scope in the control of the spread of COVID-19 in Fiji. In addition, with more than 92% of adults in Fiji vaccinated, and with the added natural immunity expected from the large number of people who were infected during the last wave on Viti Levu, we are no longer the COVID-naive population that we were before. The immunity that has been built through vaccination, and prior infection, is evidently having a significant impact in reducing severe disease in this third wave.
We will continue to work towards suppressing community transmission because we know that even if the proportion of severe cases relative to all cases is less in this third wave, a smaller percentage of severe disease in a larger number of cases will still result in a large number of sick individuals admitted to hospital, which could still overwhelm the health system’s capacity to manage. For now, we have a window of opportunity to prevent such an occurrence. This will entail adherence to COVID safe measures and having in place measures that ensure that all those vulnerable to severe disease are adequately monitored, tested, retrieved, and effectively managed in a timely manner before their conditions worsen. The latter needs the cooperation and support of community networks in formal and informal community settings and business settings, working in tandem with the Ministry. It requires that a register of vulnerable persons is established and kept in each of the settings mentioned and leaders in these settings set up a means by which vulnerable persons are checked on. If they do not feel well, they should be tested early and if positive, the nearest medical team is informed so that measures are put in place to ensure early access to medical treatment with any early signs of deterioration.
The 2 covid related deaths reported today highlight the need for such vigilance in persons with significant underlying medical conditions, especially if they are elderly.
We are seeing an increase in cases in the maritime islands and this was expected given the opening of maritime travel and the many social media postings of crowding in maritime vessels and in social gatherings. Medical Teams and supplies are being set up and being deployed to maritime islands communities reporting a surge in positive cases.
Reports of transmission to medical staff as well as staff in other workplaces are increasing, and as such isolation and quarantine measures will impact workplace outputs. The scientific basis for defining contacts and the conditions of quarantine and isolation has not changed. We note that some health authorities overseas are reducing the duration of quarantine and isolation periods. The rationale and evidence in support of these less stringent conditions are context-specific and as such we are reviewing our protocols which we will be communicating soon. All business and commercial entities need to be aware that the situation is continuously changing.
The Ministry of Health and Medical Services has also discussed with the Ministry of Education, Heritage, and Arts the current plans for school opening. We have consulted with the World Health Organisation, and UNICEF, reviewed all the evidence and taken into account our current situation, and we support the planned reopening of schools scheduled for the 4th of January 2022. We will continue to monitor our community surveillance parameters and work with the Ministry of Education to facilitate the safe opening of schools.
Our medical teams have continued to work day and night, and through the public holidays, providing healthcare to the sick, facilitating logistical requirements of medical supplies at the frontline, moving medical teams to areas of disease transmission, providing testing, continuing vaccination booster doses, protecting aged care homes, facilitating outreach to remote settings, establishing medical and community-based line lists that ensure timely follow-up of high-risk individuals, setting up intermediate care facilities with appropriate standard operating procedures, in addition to delivering normative medical care. All these activities have now escalated significantly with this new wave of the virus. At the same time, we are updating our contingency plans to be able to effectively respond to any adverse climatic weather conditions, under COVID safe conditions.
While we have also recalled targeted health staff who are on annual leave, we are very mindful of the fact that many of our staff are tired and in need of rest and recuperation. As such, senior managers have been instructed to be judicious in the deployment of staff for the various activities that need to be implemented. We have reminded all medical teams to remain professional at all times irrespective of the ongoing stressors of the pandemic and difficult individual situations. And we are committed to supporting our teams through these difficult times.
As Permanent Secretary, I am confident that our plans to mitigate this 3rd wave and the potential health impact of any severe adverse weather condition is sufficient. However, our ability to scale up these plans in a timely manner will be dictated by the impact of these natural events and will remain challenging. The need for community-wide support in terms of adherence to COVID Safe measures, instituting measures to deal with the risk of flooding and other impacts of adverse weather conditions, and facilitating ongoing vaccination is urgent and essential.
We need our people to develop and inculcate safe COVID habits into their daily living to safely navigate the current pandemic without relying on mandates and rules to do so. Enforcing settings-based measures and enforced rules are just one of many ways to promote a message to build better population-wide COVID safe habits. These COVID habits will also protect us from many other debilitating and deadly respiratory infections.