Last Updated on 38 mins by Publishing Team
COVID-19 Situation Update
Monday 03rd January 2022
| Transmission Update:
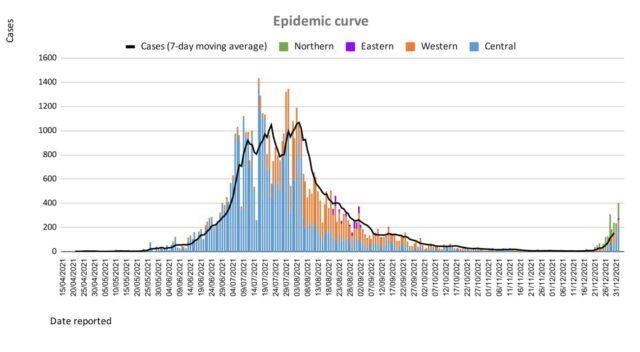
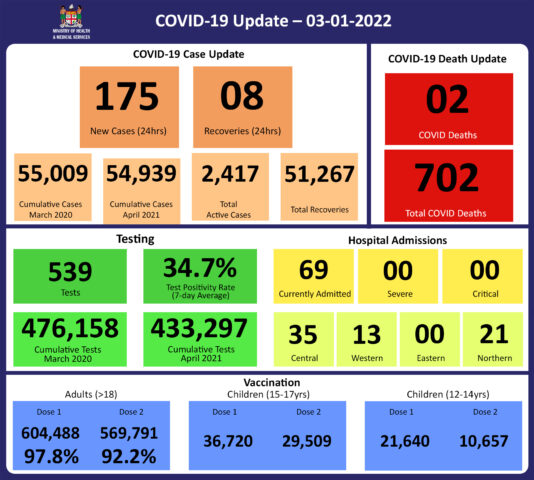
Since the last update on 01/01/2022, we have recorded a total of 580 new cases; of which 405 new cases were recorded on 02/01/2022, and 175 new cases in the last 24 hours ending at 8 am this morning. Overall, there have been 54,939 cases recorded in the 2nd wave, with 69% of the cases from the Central Division, 27% of the cases from the Western Division, and 1% of the cases from the Eastern Division, and 3% from the Northern Division. Of the 580 cases recorded since the last update, 146 cases were recorded in the Northern Division; 111 cases were recorded in the Western Division, 303 cases were recorded in the Central Division, and 20 cases in the Eastern Division. Our national 7- day rolling average is 167 daily cases calculated for 30th December 2021. |
| Deaths:
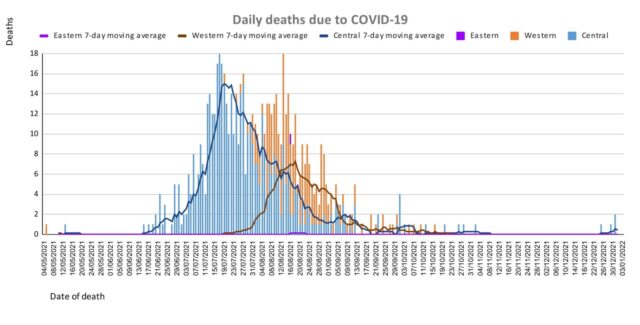
This curve depicts the daily death count by division since the 2nd wave of this outbreak that began in April 2021. Overall, the death rate graphs for the Central and Western Divisions indicate a declining trend. The differences between the Central and Western are similar to the incidence of the daily cases and are likely a reflection of vaccination levels, COVID mitigation measures, and differences in population density. There are two COVID-19 deaths to report. The first COVID-19 death to report is of a 73-year-old male from Wainibuku who died at home on 31/12/2021 in respiratory distress. He had pre-existing medical conditions and was not vaccinated. The second COVID -19 death to report is of an 84-year-old male from Kinoya who died at home on 02/01/2022 in respiratory distress. He had a significant pre-existing medical condition and was not vaccinated. There have been a total of 702 deaths due to COVID-19 in Fiji. Please note that due to the time required by clinical teams to investigate, classify and report deaths, a 4-day interval is given to calculate the 7 days rolling average of deaths, based on the date of death, to help ensure the data collected is complete before the average is reported. Therefore, as of December 30th, 2021, the national 7 days rolling average for COVID-19 deaths per day is 0.3, with a case fatality rate of 1.32%. We have recorded 621 COVID-19 positive patients who died from serious medical conditions they had before they contracted COVID-19; these are not classified as COVID-19 deaths. |
Tests
As of January 1st, rapid antigen tests conducted in the Ministry of Health and Medical Services health facilities are being added to testing numbers and test positivity calculations going back to December 23rd.
Epidemic Outlook:
The Ministry of Health continues to monitor the outbreak using indicators such as daily case numbers, hospitalizations, test positivity, and deaths.
Occupancy rates in health facilities, the occupancy rate of ICU beds, death rates, and vaccination coverage are indicators to monitor our health response capacity. While we see a low trend across indicators from our health facilities with increasing vaccination coverage for adults, 15-17-year-olds, and 12-14-year-olds in Fiji the current escalation of cases indicates a need for increased readiness and response levels for severe disease and hospitalization.
COVID-19 cases are increasing rapidly globally and especially so in Australia, and the European and Americas region, and throughout Africa. The new highly transmissible variant Omicron is contributing significantly to this increase. As such, we anticipate an increasing number of cases from border quarantine facilities. Increased and sustained surveillance and testing at our borders, communities, and maritime islands are vital to monitor and detect COVID-19 cases for early intervention.
There is an increasing number of cases in all divisions which is anticipated to continue to increase, demanding ongoing surveillance for early intervention to mitigate COVID-19 risks.
Public Advisory:
The Ministry of Health and Medical Services continues to record lower than expected hospitalization numbers despite the current resurgence in COVID-19 cases throughout Fiji. The results of positive samples sent to the Doherty Institute in Melbourne for genomic sequencing have confirmed, as expected, that we have community transmission throughout Fiji of both Omicron and Delta variants of the virus that causes COVID-19.
Omicron is vastly more infectious than Delta. As such, in keeping with what we see in other countries, the Omicron will become the dominant variant.
As Omicron spreads very fast, you should assume you are infected, and self-isolate, if you develop any cold/flu-like symptoms such as runny nose, sneezing, nasal congestion, sore throat, cough, body ache, fever. If you have any of these symptoms, please stay home to prevent infecting others, especially those who may be more at risk of severe disease. You should get tested if you can, but especially if you are at higher risk of severe disease. You are at higher risk of severe disease if you are over the age of 50, or have any significant chronic disease like heart disease, kidney disease, lung disease, diabetes, hypertension or you are obese or pregnant. If anyone in your home is at higher risk of developing severe disease, please try to isolate yourself away from them.
What to expect for the third wave
Omicron has been shown to escape immunity from infection induced by previous infection or vaccination. This means that people that have been previously infected by other variants or have been fully vaccinated with two doses of the vaccine, can get infected with Omicron. However, Omicron is more likely to cause milder disease, with data from the UK and South Africa showing that the risk of hospitalization with Omicron compared with Delta is reduced by as much as 80 percent and, once in hospital, the risk of severe diseases with Omicron is reduced by as much as 70 percent. As with previous variants, unvaccinated people are at higher risk of severe disease. With more than 92 percent of adults fully vaccinated, we expect that our high vaccination rates, plus the infection-induced immunity from the large number of people who were infected during the last wave, will help to lower the number of people that develop severe disease.
We continue to see that the majority of individuals testing positive in medical facilities are presenting for non-COVID medical problems and found to be positive while undergoing routine screening as all admissions to the hospital are currently tested for COVID-19. Also, the vast majority of cases turning positive have minimal symptoms and remain stable
However, severe outcomes will still be expected in some individuals, including those who have been immunized with two doses of the vaccine, especially people with severe underlying medical conditions and/or are over the age of 50. These factors do place a person at higher risk of severe disease, even if fully vaccinated. We have in place measures that ensure that those vulnerable to severe disease are adequately monitored, tested, retrieved, and effectively managed in a timely manner before their conditions worsen. However, we need the cooperation and support of community networks in formal and informal community settings and business settings, working in tandem with the Ministry. It requires that a register of vulnerable persons is established and kept in each of the settings mentioned and leaders in these settings set up a means by which vulnerable persons are checked on. If they do not feel well, they should be tested early and if positive, the nearest medical team is informed so that measures are put in place to ensure early access to medical treatment with any early signs of deterioration.
The current epidemic will impact our testing capacity. Many countries are struggling with testing capacity and we will be no different. As such, we continue to prioritize testing to prevent severe illness and death and to focus on transmission suppression where the risk of transmission is high.
Rapid antigen tests are very good at quickly detecting the people we need to find and isolate: those with high amounts of virus in their nose (who are therefore more infectious). These tests are more accessible than PCR tests, and the turnaround from sampling to result is much faster. However, antigen tests will miss people with lower amounts of the virus early in the disease. With the high prevalence of COVID-19 currently, if you have symptoms of COVID-19 and test negative on a single rapid antigen test, you should still assume you have COVID-19 and self-isolate.
Isolation and quarantine
As announced in previous updates, the Ministry of Health and Medical Services is aware that there are countries that have revised their isolation and quarantine protocols, based on the specific context of the outbreak in their own settings, including severely stretched testing and workforce capacity. The Ministry’s COVID-19 Taskforce has reviewed the evidence, and our specific context, and recommended changes to our isolation and quarantine protocols. The changes have been recommended based on the scientific evidence while taking into account the need to prevent severe disruption to essential services that will arise should a large number of workers be required to isolate or quarantine.
Isolation – a healthcare worker of the Ministry of Health and Medical Services who returns a positive test result will be required to self-isolate at home for 7 days, become asymptomatic, and return a negative RDT test on the 6th and 7th day before they can return to work. They will be required to maintain strict masking for the remainder of 3 days to complete the 10-day isolation requirement before they are fully discharged from isolation. In the unusual circumstances where the healthcare worker’s absence will severely debilitate the health service, processes will be put in place by the respective health care facility to ensure that a safe corridor of movement and work is created for asymptomatic healthcare workers while maintaining the full isolation requirements.
For the general public, an isolation period of 10 days for confirmed cases remains in place as before, with the case able to leave isolation without repeat testing once 10 days have passed since the start of symptoms (with at least 3 consecutive days of no symptoms) or the positive test (for asymptomatic cases). However, non-health workplaces that wish to follow the Ministry’s revised 7-day isolation SOP above will be required to cater for the testing requirement and strict masking requirement at their own cost.
Quarantine – healthcare workers of the Ministry who work in a low disease prevalence area and become a close contact of a confirmed case will be required to self-quarantine at home for 10 days with daily symptoms checking and strict COVID safe measures before they are allowed to return to work. They must be tested if they develop symptoms. However, if the healthcare worker is working in a high disease prevalence area where essential health services are at risk of being severely debilitated by a high number of healthcare workers having to quarantine or isolate, the healthcare worker will be required to return to duty at their respective health facility with strict adherence to COVID safe measures and infection prevention and control measures, undergo regular symptoms monitoring while at work, and have daily rapid antigen testing before the start of the shift. They are to immediately stand down from duties and isolate if they develop symptoms or return a positive test.
For the general public, a strict 10 days quarantine period will apply to all individuals who are close contacts of a positive case. This is the same quarantine strategy used for the Mitigation phase in the central division and the Western Division during the second wave, and so should be familiar with members of the general public.
Maritime travel restrictions
We are seeing an increase in cases in the maritime islands and this was expected given the opening of maritime travel and the many social media postings of crowding in maritime vessels and in social gatherings. Medical Teams and supplies are being set up and being deployed to maritime islands communities reporting a surge in positive cases. In view of the disease outbreak in the Northern division as well as a number of islands in the Eastern division, the following shall be implemented from Tuesday 04th January 2021:
- Travelers on boats between Viti Levu and Vanua Levu: In light of the high prevalence of COVID-19 in Viti Levu and Vanua Levu, the Ministry will not require pre-departure testing before traveling to Viti Levu and Vanua Levu. However, strict adherence to personal COVID safe measures during the travel such as mandatory masking, personal hand gel for hand hygiene and ships to ensure the soap is available throughout the trip, careFIJI app on, and passengers are fully vaccinated with 2 or more doses. Ministry officials will be closely monitoring the implementation of the new travel protocol.
- Travelers on boats from Viti Levu to Eastern division maritime islands that are currently experiencing disease outbreaks will be restricted to travelers for essential services only, for example, teachers, nurses, Government staff on official trips, those workers (and their families) who are getting posted or transferred to the islands, and permanent island residents who came to Viti Levu for the holidays and are returning to their homes without the need to come back to Viti Levu in the immediate future. This measure is to limit unnecessary population movement into the islands as the Ministry is now facing challenges in the medical evacuation of COVID cases to the main hospitals in Viti Levu as the operations of the contracted medevac providers are also affected by the current outbreak.
- Travelers on boats from the Eastern division islands to Viti Levu who have been identified as positive cases or close contacts of cases will be required to complete 10 days of isolation in their homes on the islands, be symptoms free, and with no pre-departure testing required before they are allowed to board the boat back to Viti Levu. Our team on the islands will ensure that these amended protocols are adhered to to protect the traveling population as well as the limited health care capacity on these islands.
Advice to the public on COVID safe measures
The festive season has brought about the significant movement of people as families reunite to celebrate Christmas and New Year. Gatherings have been observed where COVID-safe measures have not been followed, or people have attended while having symptoms. We ask that if you have relaxed in your observance of COVID safe measures, that you please resume now.
Always carry a well-fitted mask when you leave home, and wear it in any public indoor settings and outdoor settings where there are crowds. Avoid crowds and poorly ventilated spaces. Maintain at least 2 metres of physical distancing from others when outside your home. Wash your hands frequently with soap and water or use an alcohol-based hand sanitiser. Stay home and do not attend any gatherings if you have any symptoms of COVID-19. And get vaccinated if you are eligible and have not yet been vaccinated. And get a booster dose if you are over the age of 18, but especially if you are at higher risk of severe disease.